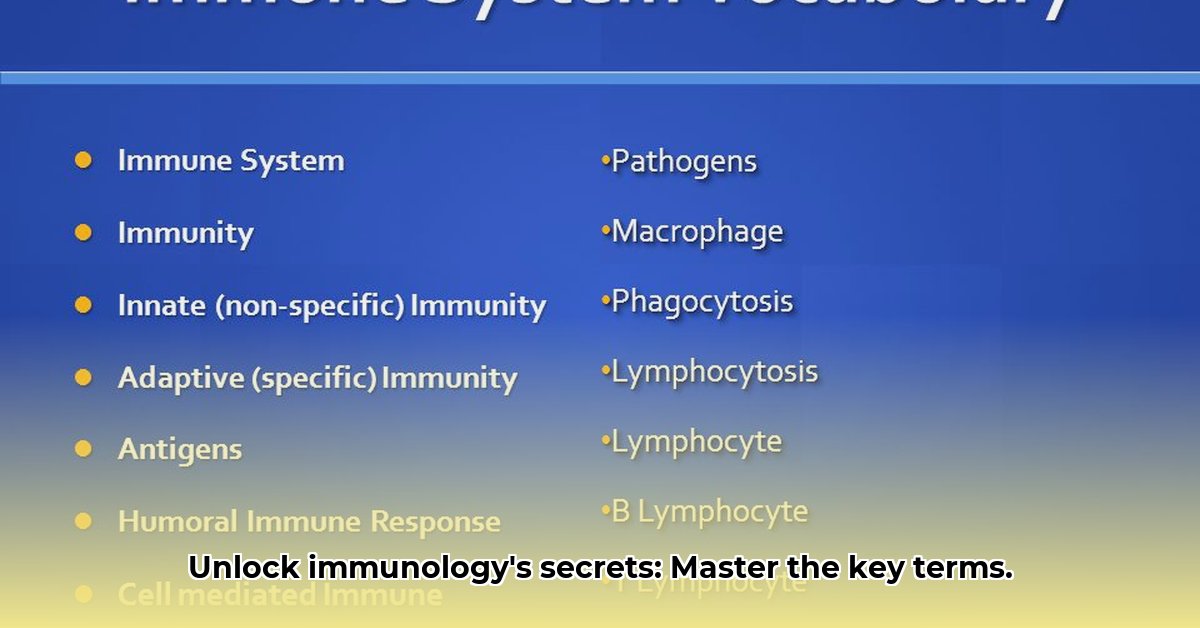
Immunology Research Vocabulary: A Comprehensive Glossary
This glossary defines key terms related to the adaptive immune response, clarifying complex concepts for researchers, students, and anyone interested in immunology. We aim for precision and accessibility, providing clear explanations without excessive technical jargon. For a broader understanding of immunological terms, see this helpful resource on immunology terms.
Affinity Maturation
- Pronunciation: ə-ˈfi-nə-tē ˌma-chə-ˈrā-shən
- Definition: A process during the adaptive immune response where B cells producing antibodies with higher affinity (binding strength) for a specific antigen are preferentially selected and expanded. This results in antibodies with increasingly stronger binding over time.
- Significance: Crucial for generating highly effective antibodies capable of neutralizing pathogens and toxins. Essential for long-term immune response and immunological memory. Defects compromise immunity.
- Example: Imagine antibodies as keys and antigens as locks. Affinity maturation refines the "keys" (antibodies) to fit the "locks" (antigens) more precisely.
Antibodies (Immunoglobulins)
- Definition: Y-shaped proteins produced by plasma cells (specialized B cells) that specifically bind to antigens. They're the primary effectors of the humoral (fluid-based) immune response.
- Significance: Neutralize pathogens by blocking infection, marking them for destruction by other immune cells (like macrophages), or directly triggering their destruction.
- Example: Antibodies act like guided missiles, targeting and eliminating specific invaders.
Antigen-Presenting Cells (APCs)
- Definition: Immune cells (including dendritic cells and macrophages) that capture antigens and present fragments (epitopes) to other immune cells, mainly T cells.
- Significance: Essential for initiating the adaptive immune response. They act as messengers, informing T cells about the presence of an invader, initiating a targeted attack.
B Cells (B Lymphocytes)
- Definition: Lymphocytes that mature in the bone marrow and differentiate into plasma cells, which produce antibodies.
- Significance: Critical for humoral immunity. Some differentiate into memory B cells, providing long-term immunity.
Clonal Expansion
- Definition: The rapid proliferation of activated B or T cells, creating many identical copies (clones) after encountering their specific antigen.
- Significance: Amplifies the number of immune cells specific to a particular antigen, ensuring a sufficient response to eliminate the threat.
Clonal Selection
- Definition: The process where only immune cells with receptors that recognize a specific antigen are activated and undergo clonal expansion.
- Significance: Ensures a focused immune response, preventing a harmful, widespread reaction.
Cytokines
- Definition: Signaling proteins that mediate communication between immune cells, regulating various aspects of the immune response.
- Significance: Control cell growth, differentiation, and activation, coordinating a successful immune response. They are the immune system's communication network.
Immunological Memory
- Definition: The long-term capacity of the immune system to remember prior encounters with pathogens, enabling a faster and stronger response upon re-exposure.
- Significance: Basis for vaccination. Provides long-lasting protection against subsequent infections.
Major Histocompatibility Complex (MHC) Molecules
- Definition: Surface proteins that present antigen fragments to T cells, initiating T cell activation.
- Significance: Essential for T cell recognition of antigens; without MHC, T cells couldn't "see" the invaders.
T Cells (T Lymphocytes)
- Definition: Lymphocytes that mature in the thymus and play key roles in cell-mediated immunity. Helper T cells coordinate the response; cytotoxic T cells directly kill infected cells.
- Significance: Central to cell-mediated immunity; they orchestrate and execute the attack against infected cells.
How to Quantify Adaptive Immune Response Kinetics in Different Antigen Types
This section explores methods for quantifying the dynamics of the adaptive immune response, integrating experimental data and mathematical modeling. Understanding these kinetics is crucial for designing effective vaccines and therapies.
Key Takeaways:
- Murine influenza models and mathematical vaccine simulations provide insights into quantifying adaptive immune response kinetics.
- Quantitative methods are essential for understanding the temporal dynamics of immune responses.
- Antibodies (IgG) and CD8+ T cell responses are pivotal in viral clearance.
- Vaccine design can be optimized by manipulating antibody production and decay rates.
- Individual variability necessitates further research to refine mathematical models.
- Long-lived plasma cells and memory B cells are crucial for lasting immunity.
Understanding Antibody Dynamics
Antibody dynamics involve multiple stages: antigen encounter, antibody production, affinity maturation, and the roles of different antibody isotypes (IgG, IgM, IgA). Analyzing this intricate process is crucial for understanding immune responses.
Quantifying Immune Response Kinetics: Influenza and Vaccines
Murine influenza models showcase the kinetics of viral clearance, highlighting the role of CD8+ T cells and antibody production. Mathematical vaccine models simulate the impact of various vaccine types on antibody dynamics and vaccine efficacy. These approaches complement each other, providing valuable insights into immune response kinetics.
Integrating Approaches for Improved Vaccine Design
By understanding the kinetics of adaptive immune responses, scientists can engineer vaccines that elicit more robust and long-lasting antibody responses. This involves considering antibody isotype, affinity, and the role of long-lived plasma cells and memory B cells. A deeper understanding of these dynamics paves the way for improved vaccine design and therapeutic strategies.